Let's Talk about Supplementation #4
Nicotine: A double-edged sword in peripheral neuropathy
Fluoroquinolone-associated disability (FQAD) is a debilitating condition characterized by persistent neurological symptoms following exposure to fluoroquinolone antibiotics. These symptoms include collagen loss, tendonitis, peripheral neuropathy, sensory disturbances, chronic pain, muscle weakness, mast cell overactivation, cognitive impairment, and autonomic dysfunction.
Today, I will delve into the topic of peripheral neuropathy, which is often associated with the use of fluoroquinolone antibiotics.
While traditionally attributed to mitochondrial toxicity or GABAergic inhibition, I found several papers (see previous posts) showing that dysregulation of cholinergic signaling—particularly prolonged upregulation of acetylcholinesterase (AChE)—plays a central role in the pathogenesis and persistence of FQAD-related peripheral neuropathy.
This post synthesizes current scientific understanding from available papers to explain how acetylcholinesterase (AChE), intracellular calcium dynamics, and muscarinic/nicotinic acetylcholine receptors (mAChRs/nAChRs) influence sensory neuron maintenance and repair, evaluates the risks and benefits of nicotine as a therapeutic agent; and discusses other therapeutic options.
First, you need a bit of explanations on how sensory neurons rely on Acetylcholine and calcium influx.
1. Fluoroquinolone-Induced Cholinesterase Upregulation and Peripheral Neuropathy
Evidence of Prolonged Cholinesterase Upregulation in the Cortex
Studies on rodents administered ciprofloxacin or gatifloxacin revealed differential regulation of cholinesterase activity across brain regions:
In the frontal cortex, both antibiotics significantly increased acetylcholinesterase (AChE) activity in a dose- and time-dependent manner, reaching maximal levels after 14 days of treatment.
In contrast, AChE activity was decreased in the hippocampus, suggesting regional specificity of fluoroquinolone neurotoxicity.
This cortical AChE upregulation is highly significant because:
The cortex regulates descending modulatory pathways to the spinal cord and peripheral nerves.
Chronic AChE overactivity leads to accelerated breakdown of acetylcholine (ACh), reducing cholinergic tone.
In the context of peripheral neuropathy, this may impair neuroprotective and regenerative signaling in sensory neurons.
Moreover, elevated AChE levels are not unique to FQAD. They are well-documented in type 2 diabetes mellitus (T2DM) and Alzheimer’s disease (AD), where they correlate with insulin resistance, inflammation, and neurodegeneration. This overlap suggests a shared pathophysiological mechanism: chronic cholinergic deficit due to AChE overactivity may underlie both metabolic and neurotoxic neuropathies.
🔍 Key Insight: Prolonged AChE upregulation in the cortex during FQAD likely contributes to a state of systemic cholinergic hypofunction, impairing central regulation of peripheral nerve health and exacerbating sensory neuron degeneration. As I indicated previously, FQAD is a disease targeting hundreds of enzymes, and any individual exhibiting weakness in the enzymes targeted by FQs will develop more severe symptoms. Here, it becomes clearly apparent that individuals with high blood glucose levels, low insulin or low acetylcholine levels are at increased risk of developing peripheral neuropathy following fluoroquinolone treatment. This may also serve as a sign to pay particular attention to the central nervous system, since if acetylcholine is downregulated, this could also have consequences for the brain (Alzheimer's) and diabetes (Type II).
2. Role of Acetylcholinesterase, Calcium, and ACh Receptors in Sensory Neuron Maintenance & Repair
A. Acetylcholinesterase (AChE): The Gatekeeper of Cholinergic Tone
AChE terminates synaptic transmission by hydrolyzing acetylcholine into choline and acetate.
Elevated AChE → reduced extracellular ACh → diminished activation of both nicotinic (nAChR) and muscarinic (mAChR) receptors.
In sensory neurons, this results in:
Loss of trophic Ca²⁺ signals via nAChRs.
Reduced activation of pro-growth pathways (e.g., PI3K/Akt, CREB).
Impaired mitochondrial function and axonal plasticity.
We are therefore in a situation where the decrease in acetylcholine caused by the upregulation of acetylcholinesterase reduces the calcium influx necessary for the regeneration of sensory neurons. But this loss of calcium influx is specific to neurons, because in other tissues affected by fluoroquinolones, the problem is the opposite, and an excessive influx of calcium instead causes mitochondrial damage and cell death, as for example in tendons.
B. Calcium Signaling: The Double-Edged Sword in Neuronal Plasticity
Calcium is essential for neuronal survival and growth, but its dysregulation leads to excitotoxicity.
In FQAD, fluoroquinolones may:
Disrupt NMDA receptor regulation via Mg²⁺ chelation (as suggested by studies showing fluoroquinolones abolish the Mg²⁺ block of NMDA channels).
Promote chronic Ca²⁺ overload via both NMDA and voltage-gated calcium channels (VGCCs), especially when combined with reduced AChE activity in some brain regions.
Simultaneously, reduced nAChR activation due to AChE upregulation removes the protective Ca²⁺ signals needed for repair.
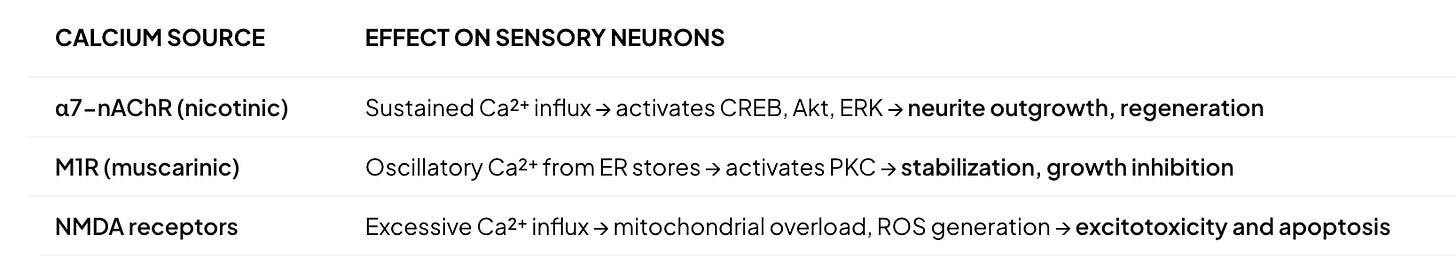
Critical Balance: The functional outcome depends on the amplitude, duration, and source of Ca²⁺:
> Low/mild oscillatory Ca²⁺ → stabilization.
> Sustained, high-amplitude Ca²⁺ (from nAChR or NMDA) → growth.
> Persistent, unregulated Ca²⁺ → neurodegeneration.